Millions of people throughout the world suffer from depression, which often doesn’t respond to standard treatments like medicine and therapy. Transcranial magnetic stimulation (TMS) therapy for depression is a unique, advanced, and non-invasive therapy that is quickly becoming popular with both doctors and patients. We’ll go over everything you need to know about TMS in this article: how it works, who it benefits, its success rate, the risks, and what to expect from TMS therapy.
What is TMS (Transcranial Magnetic Stimulation)?
Transcranial magnetic stimulation (TMS) is a medical procedure that uses focused magnetic fields to reactivate certain parts of the brain. TMS is non-invasive; therefore, there is no need for surgery, anesthesia, or electrical shocks, unlike traditional medications or electroconvulsive therapy (ECT).
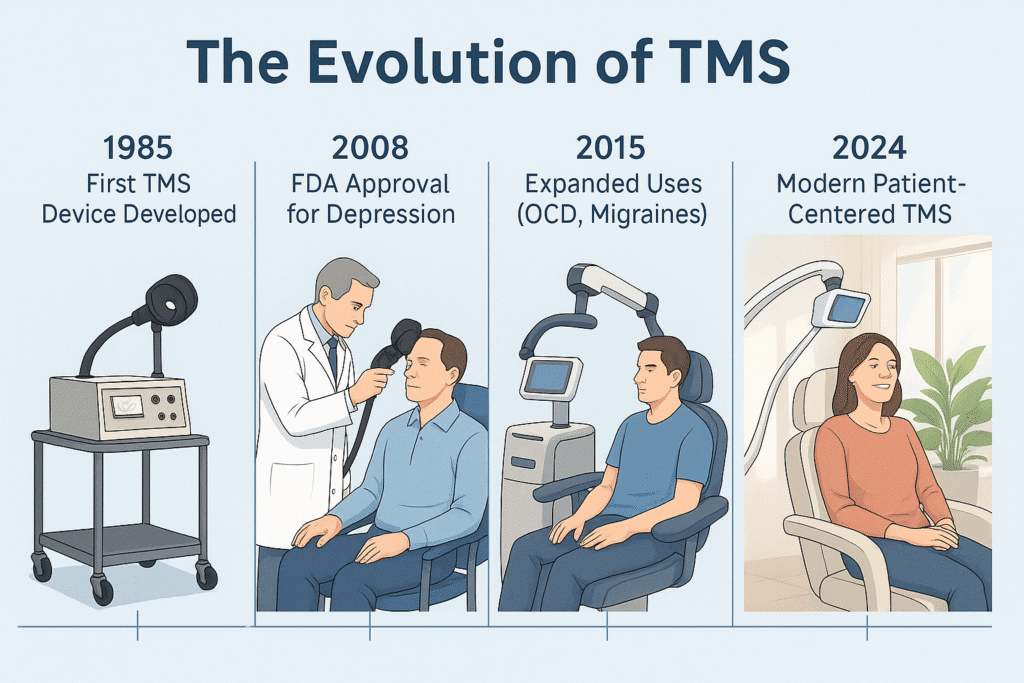
The U.S. Food and Drug Administration (FDA) first approved TMS in 2008 for people with Major Depressive Disorder (MDD) who haven’t responded to traditional treatments. Its use has grown over the past ten years to include obsessive-compulsive disorder (OCD), migraines, and quitting smoking. But depression is still its most studied and common use.
How TMS Works: A Simple Explanation of the Science
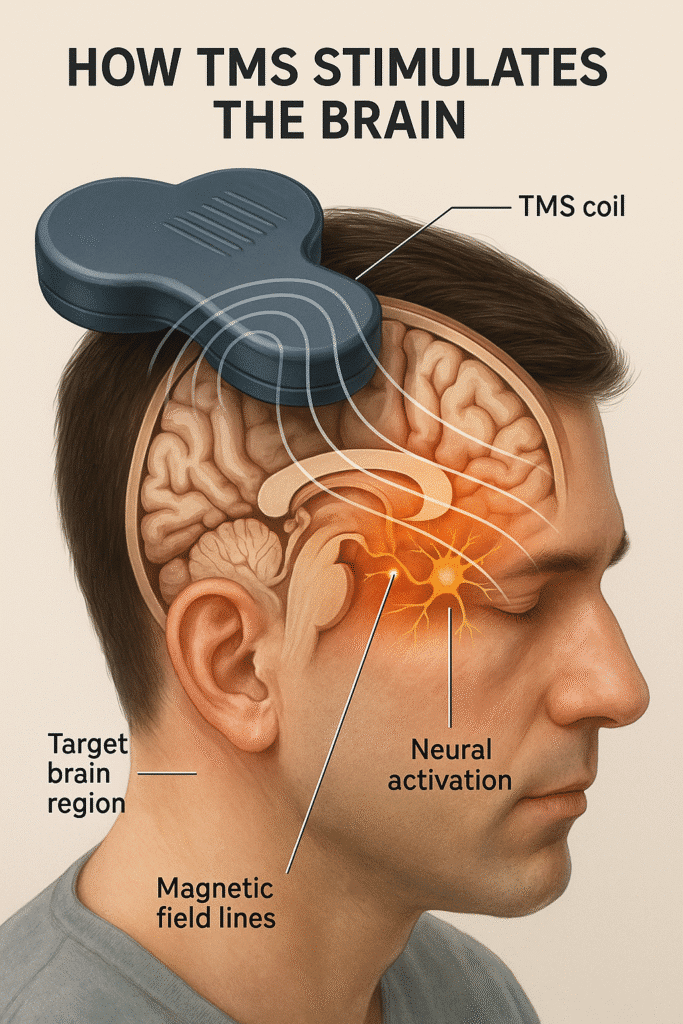
TMS primarily transmits magnetic pulses via electromagnetic coils gently applied to the scalp. These pulses activate nerve cells in the part of the brain that controls mood, most notably the left dorsolateral prefrontal cortex (dlPFC), which is often not very active in individuals with depression.
Key Features:
- No need for surgery: it is performed on the surface of your head.
- Not painful: Most patients just feel a tapping feeling during treatment.
- No anesthesia: You’ll be awake and aware the whole time.
Why does stimulating the brain help?
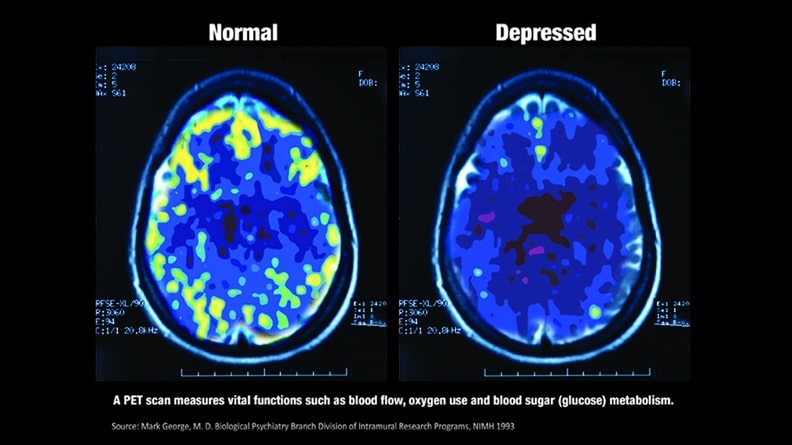
Your brain cells, or neurons, send electrical impulses to each other for communicating. Some brain circuits become less active when someone is depressed. TMS basically “restarts” these circuits, which helps bring mood control back to normal.
Who is a suitable candidate for TMS?
People over 18 with major depressive disorders who haven’t gotten better with at least one or two antidepressant drugs or therapy are the main ones who should try TMS. It works notably well for “treatment-resistant depression” (TRD).
You might be eligible for TMS if:
- You have moderate to severe depression that hasn’t gotten better with medicine or therapy.
- You can’t handle the side effects of the medicine.
- You don’t want to lose your memories or experience the risks associated with anesthesia during ECT.
- Your doctor will check to make sure you don’t have any metal implants or a history of seizures.
Care that helps you move forward
When life feels heavy or unclear, steady support matters. Bright Horizons Psychiatry offers thoughtful, practical care to help you regain balance and direction.
Book a Free ConsultWho should NOT get TMS?
People who have metal implants in their heads (such as aneurysm clips or cochlear implants), pacemakers, or a history of seizures or epilepsy should not use TMS.
How TMS Procedure looks like
Before Treatment
A psychiatrist or neurologist that works with TMS will meet with you to go over your medical history, medications, and conditions to make sure TMS is safe for you.
During a TMS Session
- Seating: You will sit in a comfy chair in the treatment room..
- Get ready: you will get earplugs because the coil can be loud.
- Coil Placement: The electromagnetic coil is softly placed against your scalp.
- Mapping: The provider finds the right area and energy level (motor threshold)..
- Stimulation: Depending on the procedure, quick pulses are given for 3 to 20 minutes.
- Sensation: You might feel tapping or slight twitching, but you can read, listen to music, or relax while you get therapy.
Care that helps you move forward
When life feels heavy or unclear, steady support matters. Bright Horizons Psychiatry offers thoughtful, practical care to help you regain balance and direction.
Book a Free ConsultAfter Treatment
You can drive and get back to your normal life right away—no time off is needed.
A full course usually has 20–30 sessions over 4–6 weeks, with 5 sessions per week.
How well does TMS work for depression?
Clinical studies and real-life experience demonstrate that TMS can help people with depression who haven’t responded to previous treatments.
What do the figures say?
- Response rates: 70–80% of patients see a big improvement.
- Remission rates: 30–35% of patients who respond to treatment achieve full remission, meaning they experience no symptoms..
- Long-term benefit: Many patients keep getting better for months or even years, especially if they keep getting therapy or medication.
How long it typically takes to see results?
Some people feel better after just a few sessions, while others see their condition become better over the course of weeks. The most benefits usually show up 2–4 weeks after finishing the whole course.
Care that helps you move forward
When life feels heavy or unclear, steady support matters. Bright Horizons Psychiatry offers thoughtful, practical care to help you regain balance and direction.
Book a Free ConsultKey advantage:
One big plus is that TMS doesn’t make you gain weight, have sexual side effects, or lose your memory like a lot of depression drugs and ECT do.
TMS Compared to Other Depression Treatments
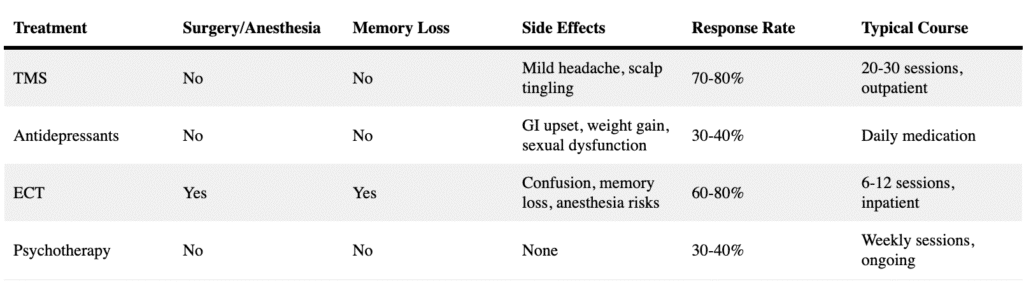
Note: It’s important to remember that TMS is commonly used with drugs and treatment, not as a replacement.
Risks and Side Effects of TMS
TMS is mostly safe and comfortable. Side effects that happen most often are minimal and go away quickly:
- The most common side effects include discomfort in the scalp or a headache.
- Twitching or tingling of the facial muscles.
- Feeling lightheaded
Over time, these symptoms normally get better. Over-the-counter pain medications can help with headaches.
Serious but rare risks:
- Seizures (risk of less than 0.01% each session)
- Hearing loss (if ear protection is not worn)
- Mania (in people with bipolar disorder—screening is important)
Your TMS Expert will go over safety with you in excellent detail and help you lower any potential risks.
What Does the Study Show?
Many big clinical trials and meta-analyses show that TMS works and is safe for treating depression.
- Numerous randomized controlled trials show TMS can substantially minimize depression symptoms in individuals with treatment-resistant depression.
- Long-term studies show that people can keep getting well with maintenance sessions or continued medication or therapy.
- Imaging studies show that TMS makes certain parts of the brain more active.
A multicenter trial including more than 300 participants revealed that about two-thirds of patients saw a measurable reduction in depressive symptoms soon after TMS, with approximately one-third achieving complete remission.
The mechanism behind TMS
It isn’t clear how TMS works exactly; however, it seems to:
- Improve neuroplasticity, which is the brain’s ability to make new connections.
- Bring back normal operation to mood circuits that aren’t working properly.
- Make the prefrontal cortex more active and blood flow better.
Transcranial magnetic stimulation for depression is changing lives and giving hope to people who think they have no other options. TMS is expected to become simpler than ever to get and perform better as research continues. Be open-minded and consult your physician to determine if TMS is a suitable option for you.
If you have questions or want to learn more about TMS, book a free consultation today.